Compliance frameworks work saving companies, including health providers, from ruin by reducing breach costs, protecting consumers and patients, and preventing the collapse of trust systems according to a Forbes article. On that note, IBM’s 2024 Cost of a Data Breach report indicates that health insurance portability and accountability act (HIPAA) compliant healthcare providers may reduce potential breaches by 30-50%. While it is difficult to streamline security operations with low budgets, there are ways for healthcare organizations to improve patient safety and ensure business continuity by focusing on inexpensive but effective strategies. Boosting security does not necessarily have to involve spending a fortune from conducting high-risk assessments to effective controls.
Inventory of the Existing Resources and Technology
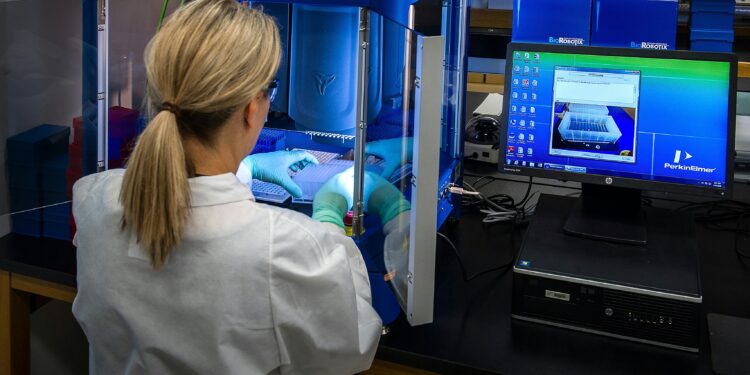
Healthcare organizations face many challenges including operating in a highly regulatory environment, vulnerable legacy devices, and tight operational budgets. Ideally, a healthcare entity should be able to hire the services of healthcare cybersecurity companies that will take care of the digital security of organizations. After all, healthcare providers hold the key to delicate personal data and life-critical systems. In the absence of a large budget, the goal of healthcare providers is, therefore, to reach security maturity without raising cost.
One way to do this is to assess the current levels of human and technological resources. Identify and prioritize the most critical assets including electronic health records (EHR) and systems and patient data storage and their biggest vulnerabilities. Implement high-impact, low-cost controls including multi-factor authentication (MFA) for all remote access and email systems. Cybercrime Magazine indicated that this is a highly effective low-cost measure that thwarts 30-50% of attacks. In addition, enforcing complex and unique passwords for all accounts ensures that the first line of defense for patient data and organizational resilience is strong. Furthermore, the principle of least privilege must be enforced meaning access rights of staff are limited in line with their job roles. Likewise, regular software updates and patching are zero-cost operational tasks that fix known vulnerabilities exploited by hackers. Staff must also undergo mandatory and recurring training so that they can recognize phishing attacks, secure data, and report incidents. In this regard, employees are also considered the first line of defense.
Optimization of Affordable Technology
Healthcare environments are complex but optimizing security does not always need expensive tools. The key is to maximize what exists and deploy high-impact low-cost solutions and align everything to the actual risks and threats in clinical and administrative workflows. For example, automation reduces operational costs and human error. By using built-in features in existing tools, compliance reporting, log collection, and initial alert triage are automated.

Where possible, tools that leverage artificial intelligence (AI) or machine learning (ML) must be used to filter out false alarms and prioritize critical security alerts. To avoid expensive hosting on-premises hardware and paid software, cloud-based solutions can be chosen. These often include built-in security features, automatic updates, and scalable resources which are more cost-effective than an on-site data center. It is also important to ensure regular, encrypted, offsite backups of all critical data. Utilize free and open source solutions like Snort or Suricata for core security functions. Self-hosted versions of open-source password vaults is another tool that can be used by healthcare providers. Instead of hiring and retaining a dedicated in-house team of security experts, an organization can outsource security operations center as a service for a set monthly fee. Outsourcing 24/7 monitoring, threat detection, and response to a managed security service provider (MSSP) is an alternative for those with limited budgets.
Adherence and Preparedness
Complying with HIPAA is non-negotiable and therefore, adequate preparation is essential to minimize the cost of a breach. Thus, it is vital to maintain clear security policies and procedures including access controls, data usage, and incident response. In the same manner, basic logging tools to maintain auditable trails of user activity on critical systems are necessary. Providers must also create a simple and documented plan on how to contain, investigate, and recover from a security incident. Exercises and simulated incidents with key staff must be undertaken to test the plan and identify weaknesses. This is because a fast response time significantly reduces the financial and reputational cost of a breach.
Security is an operational necessity for healthcare providers to adhere to HIPAA and respond promptly to the evolving threat landscape. The goal is to build operational resilience that will protect patient information and assure continuity of care in the framework of existing human resources, technology, and limited budgets.